Patients tell me all the time that they have sciatica. Many of them don’t. Sciatica can be confused with other conditions that cause low back pain or hip pain that is referred to the legs.
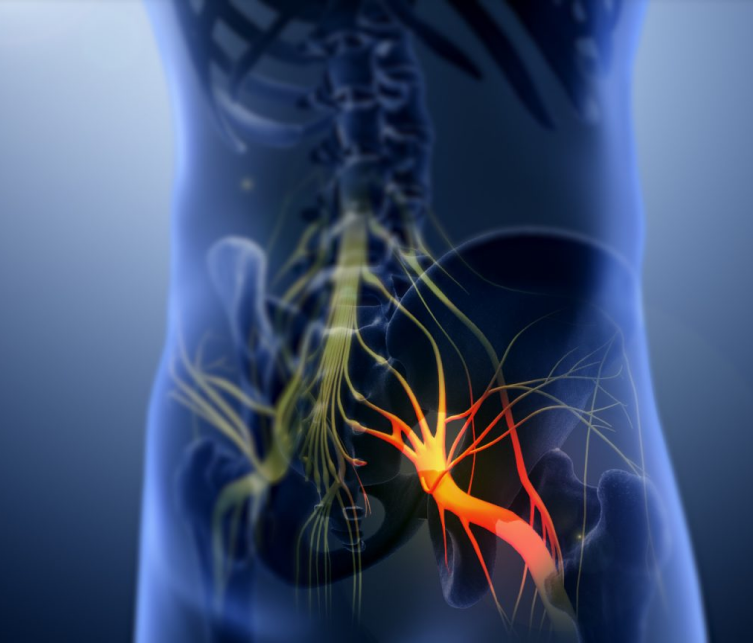
Sciatica diagnosis is fairly specific. It refers to back pain caused by a problem with the sciatic nerve. It is a large nerve that runs from the lower back spine down the back of each leg. When something injures or puts pressure on the sciatic nerve or any nerve components, it can cause pain in the lower back that spreads to the hip, buttocks, and leg. It usually only involves one leg. The pain will run down the back of the leg often going into the foot. The most common symptom of sciatica is lower back pain that extends through the hip and buttock and down one leg. The pain usually affects only one leg and may get worse when you sit, cough, or sneeze. The leg may also feel numb, weak, or tingly at times. The pain can vary widely, from a mild ache to a sharp, burning sensation, or excruciating pain. Sometimes it can feel like a jolt or electric shock. The symptoms of sciatica tend to appear suddenly and can last for days or weeks. It can also feel like a bad leg cramp that lasts for days.
Who is at risk of getting sciatica?
- Age. Age-related changes in the spine, most often seen in 30-50-year-olds. Herniated disks and bone spurs in the spine, are the most common causes of sciatica.
- Obesity. Increased body weight can contribute to the spinal changes that trigger sciatica such as accelerating arthritis or causing a herniated disk.
- Pregnancy. Women during pregnancy because of pressure on the sciatic nerve from the developing uterus.
- Occupation. A job that requires you to twist your back, carry heavy loads or drive a motor vehicle for long periods.
- Prolonged sitting. People who sit for prolonged periods or have a sedentary lifestyle are more likely to develop sciatica than active people are.
- Diabetes. It increases the risk of nerve damage.
What are the causes of sciatica?
- Degenerative arthritis of the spine
- Pinched Nerve (radiculopathy) from a disk herniation
- Foraminal stenosis. Narrowing in the opening where the spinal nerves come out.
- Spinal stenosis. Narrowing of the spinal canal.
- Piriformis syndrome
- Tumor compression (rare)
How is Sciatica diagnosed?
To determine whether you have sciatica, your doctor will ask you how the pain started and the location of the pain. You may be asked to squat, walk on your heels or toes, or raise your leg without bending the knee (called a straight leg test). These muscle tests can help your doctor determine if it is the sciatic nerve that is irritated. We may order an MRI or CT scan to confirm the diagnosis.
***If you develop a loss of bladder or bowel control, contact your doctor right away. This can be a sign of a medical emergency that requires surgery to avoid permanent damage. Fortunately, this complication is rare. Most cases of sciatica go away within a few days or weeks and cause no lasting harm.
How can you avoid Sciatica?
It’s not always possible to prevent sciatica, and the condition may recur.
- Exercise regularly. To keep your back strong, pay special attention to your core muscles — the muscles in your abdomen and lower back that are essential for proper posture and alignment.
- Maintain proper posture while sitting. Choose a seat with good lower back support, armrests and a swivel base. Consider placing a pillow or rolled towel in the small of your back to maintain its normal curve. Keep your knees and hips level.
Use good body mechanics when lifting.
- When you lift something heavy, let your lower extremities do the work.
- Dont bend your back.
- Move your back straight up and down.
- Keep your back straight and bend only at the knees.
- Hold the load close to your body.
- Avoid lifting and twisting simultaneously.
- Find a lifting partner if the object is heavy or awkward.
How is Sciatica Treated?
- Medications. Anti-inflammatories (NSAID’s, Aspirin), muscle relaxants (tizanidine, cyclobenzaprine), Opioids, Tricyclic antidepressants (Amitriptyline), or Anti-seizure medications (gabapentin, pregabalin)
- Medications. Anti-inflammatories (NSAID’s, Aspirin), muscle relaxants (tizanidine, cyclobenzaprine), Opioids, Tricyclic antidepressants (Amitriptyline), or Anti-seizure medications (gabapentin, pregabalin)
- Steroid injections. This involves injection called an epidural. Corticosteroids help reduce pain by suppressing inflammation around the irritated nerve. Steroids can also be replaced with a homeopathic injection
- Surgery. Usually reserved for when the compressed nerve causes significant weakness, loss of bowel or bladder control, or when you have pain that progressively worsens or doesn’t improve with other therapies. Surgeons can remove the bone spur or the portion of the herniated disk that’s pressing on the pinched nerve.